Chronic Pain Unveiled: Implantable Electrodes Illuminate the Secrets of Chronic Pain

Decoding Chronic Pain: Groundbreaking Brain Study Reveals Unseen Agony
In a groundbreaking study published in Nature Neuroscience, scientists have unlocked a new level of understanding in the realm of chronic pain. By implanting electrodes into the brains of four individuals suffering from persistent pain, researchers were able to capture detailed insights into the complexities of this debilitating condition. The findings, revealed on May 22, not only shed light on the invisible agony experienced by chronic pain sufferers but also offer promising avenues for curbing its impact.
Chronic pain affects an alarming number of individuals worldwide, surpassing diagnoses of diabetes, depression, and high blood pressure in the United States, as reported in JAMA Network Open on May 16.
Its enigmatic nature, influenced by a multitude of factors including the body, brain, context, emotions, and expectations, has long confounded experts, rendering it challenging to treat effectively. However, a potential breakthrough has emerged through the novel approach of electrical brain stimulation.
Revolutionary Electrode Implants Illuminate the Complexity of Chronic Pain, Paving the Way for Targeted Treatments
As part of a pioneering clinical trial at the University of California, San Francisco, researchers surgically implanted electrode wires into the brains of four volunteers suffering from chronic pain. These electrodes served a dual purpose, enabling the monitoring and stimulation of nerve cells in two specific brain regions: the orbitofrontal cortex (OFC) and the anterior cingulate cortex (ACC).
Although the OFC was not previously regarded as a primary influencer of pain, its rich neural connections to pain-related areas, including the ACC, suggested its potential involvement in pain perception.
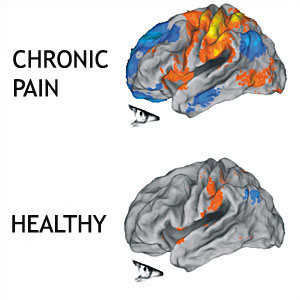
Before exploring brain stimulation as a potential treatment, researchers sought to gain insight into how chronic pain impacted brain activity. Over a period of 3 to 6 months, the implanted electrodes diligently monitored the participants’ brain signals as they went about their daily lives. During this time, the volunteers recorded their pain levels multiple times a day using standardized scales. Leveraging advanced machine learning techniques, the research team successfully linked each individual’s pain ratings to specific brain activity patterns, ultimately identifying unique signatures associated with chronic pain.
While the patterns exhibited considerable individual variation, there were notable overlaps. Particularly, brain activity in the OFC, located at the front of the brain behind the eyes, correlated with the participants’ chronic pain levels. Intriguingly, unexpected pain patterns emerged, such as recurring fluctuations on a roughly three-day cycle in two of the volunteers.
The identification of OFC brain activity as a potential biomarker for chronic pain has significant implications. Not only can it aid doctors in tracking treatment responses, but it also presents new targets for therapeutic interventions.
Neuroscientist Chelsea Kaplan of the Chronic Pain and Fatigue Research Center at the University of Michigan in Ann Arbor emphasized the importance of expanding this research beyond the study’s limited sample size, which consisted of individuals with pain from a stroke and phantom limb pain after a leg amputation.
The potential applications of this discovery extend beyond diagnosis and treatment. If common brain activity patterns can be established across individuals with chronic pain, they may serve as objective measures of pain in individuals who cannot communicate, including those in nonresponsive states like locked-in syndrome.
However, the true goal of identifying reliable markers of chronic pain extends beyond simple diagnostics. Study coauthor Prasad Shirvalkar, a neurologist at UCSF, emphasized that the purpose is to guide treatment and make patients feel truly seen. Currently, Shirvalkar and his colleagues are conducting a clinical trial involving brain stimulation in treating chronic pain, viewing the identified biomarker as a crucial tool in enhancing patient care.
As the veil of chronic pain is gradually lifted, this groundbreaking research opens up new avenues for targeted treatments and provides hope for treating chronic pains.



